Acute Kidney Injury
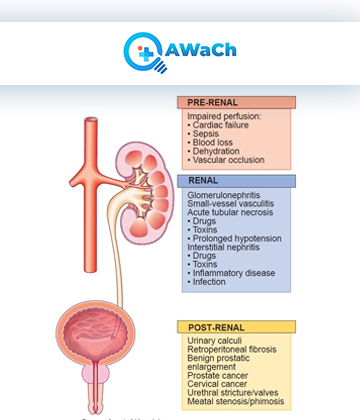
Acute kidney injury (AKI), previously known as acute renal failure, represents a medical emergency and encompasses a wide range of damage to the kidneys
(AKI) Acute kidney injury occurs when kidney function rapidly deteriorates, leading to an inability to maintain fluid, electrolyte, and acid-base balance. It contributes to increased morbidity and mortality. The severity of AKI results in significant healthcare costs. Consequently, there is a heightened focus on identifying new biomarkers for AKI. Detecting AKI earlier would ultimately preserve lives, improve patients' quality of life globally, and reduce healthcare system expenses.
What is Acute Kidney Injury (AKI) ?
In AKI, the underlying pathophysiology features a complex interaction between predisposing chronic illnesses, haemodynamic disturbances, nephrotoxic insults, and inflammatory responses, resulting in tubular cell injury and, ultimately, a reduction in glomerular filtration rate. Cardiovascular disease associates acute kidney injury (AKI) with heightened morbidity and mortality. In 2005, a landmark study of 71 children undergoing cardiac surgery showed that urine Neutrophile Gelatinase-Associated Lipocalin (uNGAL) and plasma NGAL (pNGAL), assessed 2 hours after cardiopulmonary bypass, had a high diagnostic accuracy for AKI (defined as a ≥50% increase in creatinine from baseline).
uNGAL’s sensitivity was 100% with an area under the receiver-operating characteristic curve (AUC) of 0.998, and pNGAL’s sensitivity was 70% with an AUC of 0.906. These promising results led to further studies of NGAL in cardiogenic shock, contrast induced nephropathy (CIN), heart failure (HF), sepsis, and critical illness. In critical illness, septic patients face a significantly heightened risk of AKI. In a multicenter study that included patients presenting to the emergency department with suspected sepsis, pNGAL (plasma neutrophil gelatinase-associated lipocalin) exhibited a strong predictive capacity for AKI with an AUC of 0.82, surpassing the AUC of 0.73 observed for creatinine.
Due to the use of serum creatinine and urine output to fulfill diagnostic criteria, the clinical benefits of promptly and definitively diagnosing AKI have not been fully realized. These restrictions often lead to diagnostic delays, potential classifications of actual injury status, and provide little information regarding underlying cause. Novel biomarkers of damage have shown ability to reflect ongoing kidney injury and help further refine existing Risk, Injury, Failure, Loss, End-stage kidney disease (RIFLE) and Acute Kidney Injury Network (AKIN) diagnostic criteria.
- “Acute Kidney Injury (AKI), once known as acute renal failure, is a medical emergency involving a wide range of kidney damage.”
- “AKI occurs when kidney function rapidly deteriorates, leading to an inability to maintain crucial fluid, electrolyte, and acid-base balance in the body.”
- “This condition significantly contributes to increased morbidity and mortality rates and places a substantial financial burden on global healthcare systems.”
- “The urgent need for identifying new biomarkers for AKI is emphasized by their potential to detect this condition earlier, ultimately saving lives, improving patients’ quality of life, and reducing healthcare costs.”
Strength:
Acute Kidney Injury (AKI) poses a complex challenge due to its multifaceted pathophysiology, involving a convergence of predisposing chronic illnesses, hemodynamic disturbances, nephrotoxic insults, and inflammatory responses. These factors collectively lead to tubular cell injury and a subsequent reduction in glomerular filtration rate. Notably, AKI is intricately linked with cardiovascular disease, amplifying the risks associated with morbidity and mortality. Research has demonstrated the potential of biomarkers like urine Neutrophil Gelatinase-Associated Lipocalin (uNGAL) and plasma NGAL (pNGAL) to provide early diagnostic accuracy for AKI, further emphasizing the importance of innovative diagnostics in addressing this condition.
Advantages:
The use of novel biomarkers such as Neutrophil Gelatinase-Associated Lipocalin (NGAL) has opened new avenues for the early detection and management of Acute Kidney Injury (AKI). These biomarkers exhibit high sensitivity and specificity, enabling prompt intervention and improved patient outcomes. By surpassing the limitations associated with conventional diagnostic criteria, including serum creatinine and urine output, these biomarkers offer a more comprehensive understanding of ongoing kidney injury, thus enhancing the accuracy of diagnoses and refining existing diagnostic criteria like Risk, Injury, Failure, Loss, End-stage kidney disease (RIFLE) and Acute Kidney Injury Network (AKIN).
Recognitions:
The pivotal role of innovative biomarkers in the early detection and diagnosis of AKI has garnered recognition and research interest within the medical community. Studies showcasing the diagnostic accuracy of biomarkers like (NGAL) in various clinical scenarios, including cardiogenic shock, contrast-induced nephropathy (CIN), heart failure (HF), sepsis, and critical illness, have propelled the adoption of these tools as valuable assets in the management of AKI. Their potential to reduce diagnostic delays and misclassification of injury status positions them as noteworthy contributors to the field of nephrology.
Innovation:
The development and utilization of novel biomarkers like Neutrophil Gelatinase-Associated Lipocalin (NGAL) represent a significant stride in addressing the challenges posed by Acute Kidney Injury (AKI). These biomarkers, known for their heightened sensitivity and early detection capabilities, offer a promising approach to enhancing patient care and reducing the impact of AKI on both individuals and healthcare systems. Their integration into clinical practice signifies a commitment to advancing diagnostic methodologies for improved AKI management.
