Smartphones in Healthcare !
October 1, 2022
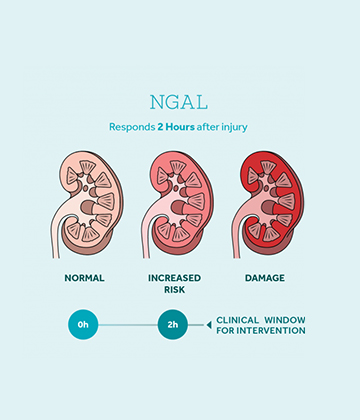
NGAL: A Sensitive and Early Biomarker for Acute Kidney Injury
October 1, 2022Did you know that, almost 30% of all hospital admissions fall in a wide definition of Acute Kidney injury (AKI) and 10% of the population worldwide is affected by Chronic Kidney Disease (CKD). Moreover, CKD is associated with the world’s two top most killers, Diabetes and Hypertension! If the above-mentioned numbers are extrapolated to the Indian population, then it translates into a huge medical burden. In a developing country like India, where the awareness about kidney disease is low, there is an immense social, psychological and financial impact of kidney failure on the patients and their family. The socio-economic impact of kidney failure (renal failure) and its aftermath are huge. The cost of getting a hemodialysis (~12 dialysis/month) could be around INR 20,000-50,000 per month, whereas for peritoneal dialysis the cost could range between INR 30,000-60,000 per month. Moreover, a kidney transplant could cost millions of rupees. Apart from this, other recurring costs per month for a kidney patient may range from INR 10,000-20,000 depending upon the condition of the patient. A financially average middle class person in India cannot afford these expensive treatments. This problem is further compounded by the fact that kidney failure is incurable and the treatment becomes a life-long expense. This situation puts a perennial load on the patient and his/her family. This financial burden is the main reason why only 2-3% of the kidney failure patients in India get the proper diagnosis and treatment. A rise in the cases of kidney failure is mainly attributed to the limitations of current diagnostic tools for an early diagnosis of kidney injury.
The loss of kidney function that defines AKI and CKD, is routinely diagnosed by measurement of serum creatinine (SCr) levels and estimated glomerular filtration rate (eGFR). However, there are certain limitations associated with these methods.
a. The eGFR and SCr levels are not linearly interdependent.
b. SCr is a slow responding molecule towards the commencement of the kidney injury.
c. SCr levels are also affected by many non-renal aspects such as age, race, gender, muscle mass, drug metabolism, protein intake, perioperative fluid administration, and hydration status.
Among the most recent sensitive biomarkers suggested for AKI, the molecule called Neutrophil Gelatinase-Associated Lipocalin (NGAL) was found to be suddenly up-regulated during the early stages of kidney injury. In contrast to the traditional markers like SCr, this rapid response enables NGAL to potentially identify kidney injury at a much earlier stage. This suggests that NGAL as a biomarker for kidney injury could prove to be better in comparison to SCr and eGFR. However, a number of factors define whether a diagnostic solution would effectively reach the masses and a timely medical intervention for kidney injury could happen. Few of these defining factors are, the availability and cost of this diagnostic method, its sensitivity and stability and requirements for a sophisticated laboratory infrastructure and technician skills to conduct the test. A point-of-care diagnostic solution based on estimation of NGAL levels in patients susceptible to kidney injury, that is easy-to-use, highly sensitive/accurate, with no specific infrastructural requirements and at the same time cost-effective, could be a reliable and effective diagnosis for early diagnosis and management of AKI.